Chronic Kidney Disease in Dogs
Adobe Stock/Alan
When you take your dog for their yearly vet exam, you might wonder why the vet would recommend running a screening blood panel and urinalysis when your pet seems to be perfectly healthy. In this situation, your vet is doing their best to uncover the onset of conditions that haven’t become obvious yet. A perfect example of one of these conditions is kidney disease in dogs.
Acute (sudden onset) kidney disease often presents with obvious illness, but chronic kidney disease in dogs appears over time—and the initial signs and symptoms may go unnoticed.
Early diagnosis and intervention are vital to managing the disease and maintaining your dog’s comfort and well-being.
Key Takeaways
- Kidney disease can sometimes be present before obvious symptoms are noticed by pet parents.
- Initial signs often include increased drinking and increased urination, lethargy, picky appetite, or weight loss—all of which can also be present in many other conditions.
- Blood work and urinalysis are the basic diagnostic tests used to diagnose kidney disease in dogs, but other tests may also be needed during the diagnostic process.
- Kidney disease is not curable and is usually progressive, but it can be medically managed in many patients to improve quality of life.
What Is Chronic Kidney Disease in Dogs?
Dogs have two kidneys, which are vital for maintaining life’s day-to-day processes. They have a variety of functions, the foremost of which is to filter and excrete toxins and waste from the body. Other tasks of the kidneys include regulating fluid, mineral, and electrolyte balance; conserving water and certain blood proteins; maintaining blood pressure; and producing red blood cells.
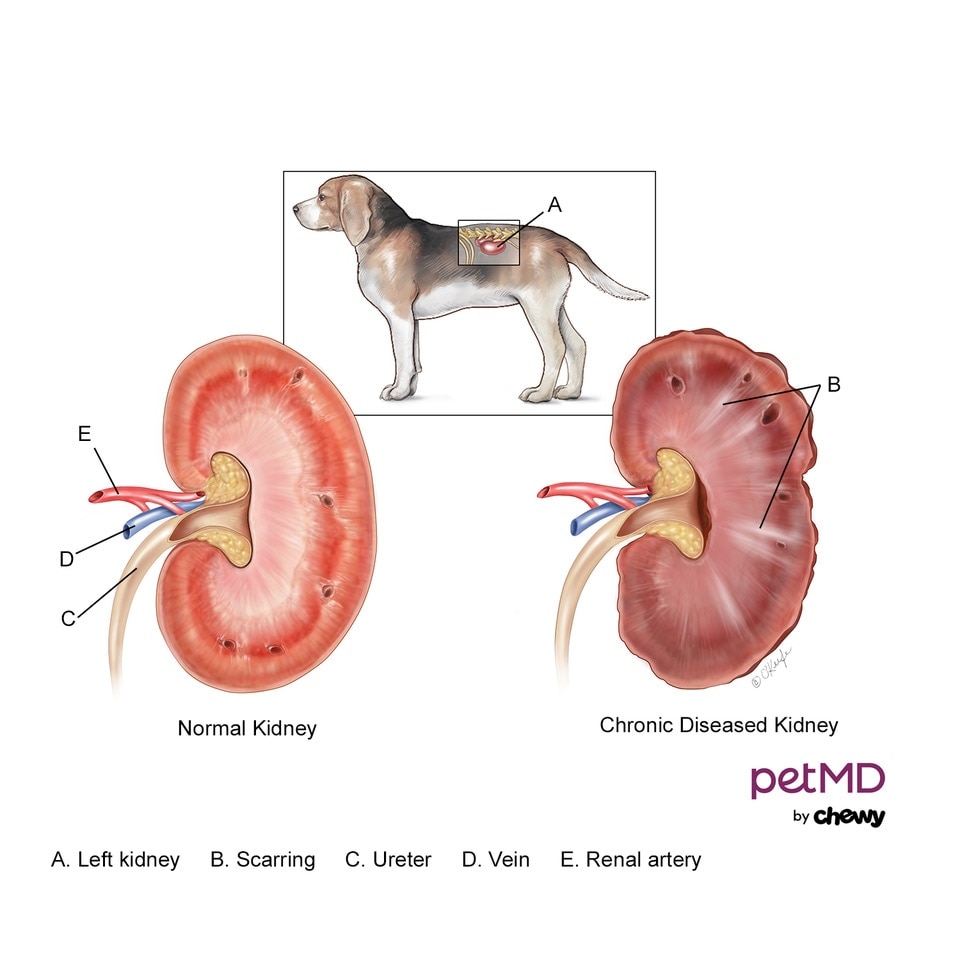
Click here to download this medical illustration.
Many causes are associated with progressive loss of kidney function; unfortunately, once lost, the damage is irreversible. As a result, unfiltered waste products and toxins build up in the bloodstream, leading to a generalized state of nausea and malaise. When left untreated or unmanaged, a dog’s quality of life suffers.
Chronic kidney disease (CKD) in dogs is a progressive disease that has often been present for some time before it is diagnosed. It progresses at a unique rate for each patient, which makes it difficult to predict. It is typically classified into four IRIS stages I–IV, based on laboratory values and clinical signs (symptoms).
Symptoms of Chronic Kidney Disease in Dogs
Dogs typically won’t experience any symptoms until the kidneys have lost about 75% of their functioning capacity. The higher the stage (meaning the greater the extent of kidney disease present), the more symptoms may be exhibited. Symptoms may also worsen in severity and complexity as the disease progresses.
Symptoms of kidney failure in dogs vary and may include:
-
Anemia (low red blood cell count)
-
Changes in urine output, usually increased
-
Decreased appetite
-
Dehydration
-
Increased thirst
-
Muscle wasting
-
Nausea
-
Oral ulcerations (sores in the mouth) and bad breath
-
Pale gums
-
Poor coat appearance
-
Sporadic vomiting
-
Vision loss, often attributed to secondary hypertension (high blood pressure)
-
Weakness and lethargy
-
Weight loss
Causes of Chronic Kidney Disease in Dogs
Chronic renal failure by definition is a disease that occurs over a period of time; it is an ongoing, progressive, and irreversible process where, for many dogs, the cause remains unknown despite extensive testing.
Sometimes chronic kidney disease in dogs develops after a serious kidney injury, such as from a severe infection (e.g., leptospirosis, tick-borne disease, or pyelonephritis aka kidney infection), heatstroke, envenomation (from a venomous bite or sting), or the ingestion of toxic substances like antifreeze, NSAIDs (ibuprofen), or certain antibiotics.
Chronic kidney disease is also associated with certain types of immune-mediated diseases or cancer.
Dogs breeds commonly prone to CKD include:
How Veterinarians Diagnose Chronic Kidney Disease in Dogs
A veterinarian will start with a physical exam, blood work, and a urinalysis to look specifically at values such as:
-
Blood urea nitrogen (BUN): Higher values may be correlated with kidney failure
-
Calcium: Elevated levels, though not as common, are often seen as the disease advances.
-
Creatinine (Cr or Creat): Indicator of the kidney’s ability to filter wastes from blood
-
Electrolytes: Sodium, potassium, chloride
-
Phosphorus: Higher phosphorus levels may be seen with chronic kidney disease
-
Red blood cell count: Low red blood cell counts are often seen secondary to more severe chronic kidney disease
-
Symmetric dimethylarginine (SDMA): An indicator used for early detection of kidney disease
-
Urine specific gravity: Determines the kidney’s concentrating ability. Usually, the lower the number, the more diluted the urine. This may indicate kidney disease, since a healthy kidney should be able to resorb water to concentrate urine to prevent dehydration.
Your veterinarian may also recommend additional tests such as:
-
A urine protein to creatinine (UPC) ratio to determine how much protein is lost in the urine (termed proteinuria)
-
A urine culture, as dogs with chronic kidney disease are more likely to acquire urinary tract infections
-
A blood pressure evaluation, as dogs with chronic kidney disease often have hypertension (high blood pressure)
-
Radiographs or abdominal ultrasound to screen for kidney stones, tumors, or infarcts (areas of dead tissue)
-
Kidney biopsy, in very rare cases
Treatment of Chronic Kidney Disease in Dogs
Chronic kidney disease in dogs is a manageable but incurable disease—since by the time a dog is symptomatic, irreversible damage has already occurred.
Recommendations based on the stage of CKD will be tailored to match your dog’s needs, with dogs in Stage III or IV warranting greater care and therapy than dogs in Stage I or II. Common therapies for chronic kidney disease include medications, diet, and fluid therapy, along with treatment for any underlying condition or inciting factors.
Medications such as Cerenia, ondansetron, or omeprazole can help treat nausea, vomiting, and lack or loss of appetite. Additionally, appetite stimulants such as capromorelin and mirtazapine may be recommended.
Most vets will prescribe dietary management with a balanced diet that is lower in protein, salt, and phosphorus and is alkalinized to help combat side effects associated with CKD. Recommended diets typically include:
Fluid management is essential. Fluids may be administered to flush out toxic waste substances from the bloodstream and improve hydration. They may be given intravenously in the hospital or subcutaneously (underneath the skin) at home. Your dog should have access to fresh water at all times—a water fountain can be an especially important item to add to your home.
Management of Chronic Kidney Disease in Dogs
Chronic kidney disease is a serious, lifelong condition that requires ongoing care and monitoring, as symptoms continue to develop. Dogs with CKD require more frequent veterinary visits and testing than others, and at all stages of CKD, quality of life should be assessed as symptoms change.
Be sure to adhere to your veterinarian’s recheck guidelines and continue all medications and diet as recommended; many will be required for life.
Depending on the circumstances, certain measures can help keep your dog comfortable and offer a good quality of life for as long as possible. Similar treatment and medications to those outlined above also are applicable for long-term management of chronic kidney disease in dogs, such as:
-
Dietary supplements such as Azodyl, a pre/probiotic, that can help decrease waste products not eliminated by the kidneys.
-
Other supplements, such as aluminum hydroxide and Epakitin, that are geared to aid with high phosphorus levels; or potassium supplements like Renal K+ that can help with low potassium levels
-
Anti-nausea and anti-emetic (anti-vomiting) medications can be prescribed as needed for dogs who experience intermittent vomiting and lack of appetite.
Chronic Kidney Disease in Dogs FAQs
How long can a dog live with kidney disease?
Chronic kidney disease is progressive; however, it’s difficult to anticipate the degree and timing of the progression. Some dogs can live for years with proper veterinary care and management, while others may have to be euthanized shortly after diagnosis.
How fast does kidney disease progress in dogs?
The progression of chronic kidney disease in dogs varies, taking weeks to years for symptoms to be noticeable. Once known, though, it is estimated that 75% loss of kidney function has already occurred, and the damage is irreversible. Depending on the underlying cause and the stage of disease at diagnosis, some dogs will decline much faster than others.
Frequent checkups and routine veterinary visits can help detect CKD sooner, which will ensure your dog’s comfort and garner an overall better quality of life.
