Pancreatitis in Dogs: Signs, Causes and Treatment
intek1/iStock / Getty Images Plus via Getty Images
What Is Pancreatitis in Dogs?
The pancreas is an organ in the abdominal cavity.
One of its roles is producing digestive enzymes, which help break down food products. When this normal process goes awry, the pancreas can become inflamed. This is a condition called pancreatitis.
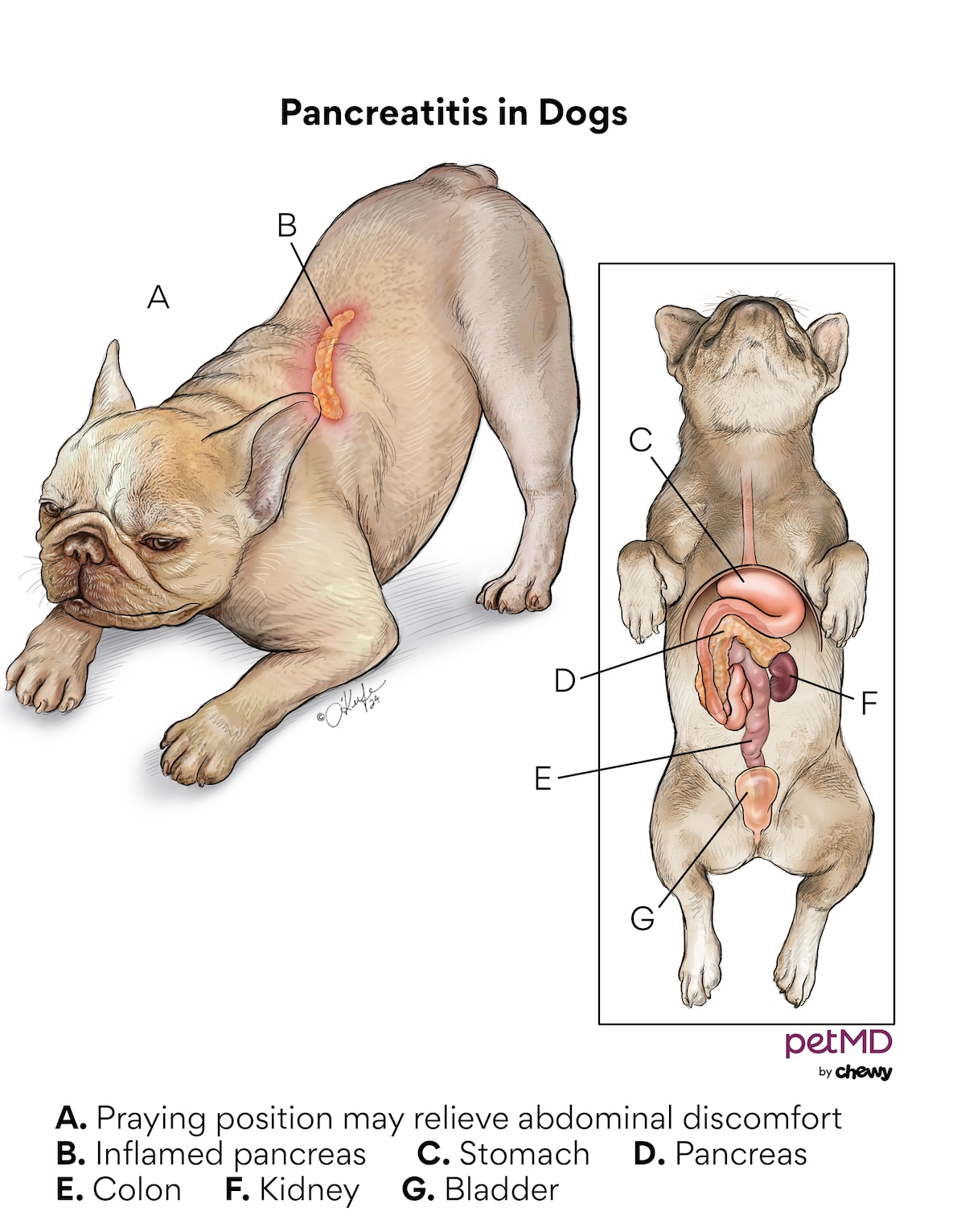
Pancreatitis in dogs is an inflammatory reaction within the pancreas that can result in abdominal pain, inappetence, and vomiting.
Affected dogs may display a praying position. In this position, the dog will raise their hind end in the air and bow their head down towards their front legs.
Click here to download this medical illustration.
This position relieves abdominal discomfort that’s associated with an inflamed pancreas. Dogs with pancreatitis often experience significant dehydration since they are vomiting.
The inflammation results from the inappropriate, early activation of an enzyme within the pancreas, which causes the pancreas to digest itself.
If left untreated, pancreatitis in dogs can become chronic and lead to weight loss and lethargy.
Seek prompt veterinary care if you think your dog may have pancreatitis. Early intervention is critical in helping dogs feel better and in preventing worsening of symptoms.
Health Tools
Not sure whether to see a vet?
Pancreatitis Symptoms in Dogs
Pancreatitis can present as a sudden-onset (acute) illness or as a more long-term (chronic) illness.
A dog that has acute pancreatitis will have more serious clinical signs, such as:
-
Severe lethargy
-
Abdominal pain
-
Persistent vomiting
-
Diarrhea
-
Severe dehydration
A dog with chronic pancreatitis is typically not as sick. The clinical signs may include:
-
Lethargy
-
Decreased appetite to not eating at all
-
Weight loss
-
Abdominal pain and/or vomiting
In general, chronic pancreatitis in dogs is not as common as acute pancreatitis.
Dogs with chronic pancreatitis can suddenly develop worsening pancreatitis. This is a situation where chronic pancreatitis presents acutely.
What Are the Signs of Worsening Pancreatitis in Dogs?
Pancreatitis can worsen quickly if treatment is not started promptly after symptoms first begin.
Dogs with worsening pancreatitis are often severely dehydrated, lethargic and weak, and in pain.
Dogs who showed some interest in food may not eat at all if their condition is advancing. If a dog’s pancreatitis is worsening, hospitalization and supportive care is needed.
Causes of Pancreatitis in Dogs
Typically, a dog that’s diagnosed with pancreatitis likely ate a high-fat meal or got into the garbage. Unfortunately, this is not the most common cause of pancreatitis. Most cases of pancreatitis in dogs are idiopathic (can’t be determined).
Some breeds are more prone to the development of pancreatitis, as well as dogs taking certain medications.
Miniature Schnauzers are a predisposed breed due their tendency to have problems with high blood triglyceride levels. Another example is the English Cocker Spaniel.
Immune-mediated diseases—which result from abnormal activity of the immune system—are seen at a higher frequency in this breed, and the immune system attacking the pancreas is no exception.
Some chemotherapy medications and antibiotics can cause inflammation of the pancreas.
How Do Vets Diagnose Pancreatitis in Dogs?
Disease of the pancreas can be difficult to identify. The signs of illness are not specific to the pancreas, and routine blood tests are often not helpful.
However, there are pancreatic-specific blood tests that can be performed when a veterinarian has a high suspicion of pancreatitis. Unfortunately, even these special tests are not 100% accurate.
Abdominal X-rays are also not very helpful in diagnosing pancreatitis in dogs.
However, in a vomiting patient, it’s important to take X-rays to rule out a potential foreign-body obstruction of the stomach and/or intestine (something your dog ate, like a squeaker out of a toy).
The best method to image the pancreas is via abdominal ultrasound.
However, the tissue of the pancreas must be abnormal enough to visualize using the ultrasound.
This is more common in dogs with acute, severe pancreatitis, compared to those with chronic, mild pancreatitis.
Overall, blood testing and abdominal ultrasounds are better in helping to diagnose pancreatitis in dogs when it’s a acute and severe case.
Treatment of Pancreatitis in Dogs
Treatment of pancreatitis in dogs is primarily supportive care regardless of whether the patient has acute or chronic pancreatitis.
Treatment for pancreatitis may include the following:
-
Intravenous (IV) fluid and electrolyte support
-
Antinausea medication(s)
-
Stomach-protectant medications
-
Nutritional support in the form of a feeding tube
-
Antibiotics (sometimes)
-
Immunosuppressants (in chronic cases)
-
A bland, low-fat diet is recommended during recovery (this may be a home-cooked and/or home-prepared diet)
How long treatment lasts for depends on how severe the symptoms were when the dog arrived at the veterinary hospital and how long symptoms have been present.
A dog with very mild pancreatitis may be treated on an outpatient basis, while dogs with severe pancreatitis require hospitalization.
Likewise, the cost of treating pancreatitis varies based on severity. Pet parents can expect to pay anywhere from $500 to $5,000 for treatment.
A permanent diet change may be recommended, especially in predisposed breeds or dogs with a history of pancreatitis.
Recovery and Management of Pancreatitis in Dogs
The prognosis for dogs with pancreatitis ultimately depends on the severity of the illness.
A dog with severe pancreatitis has a poor to grave overall prognosis, thus a higher risk of loss of life.
Patients with mild pancreatitis generally recover within a week or two. To ensure your dog’s comfort during recovery, follow your veterinarian’s instructions closely for prescription medications and provide your dog a quiet space to rest in.
Some dogs may experience multiple bouts of mild pancreatitis during their lives and benefit from a strict low-fat diet, such as Blue Buffalo Natural Veterinary Diet Gastrointestinal Support Low Fat Dry Dog Food, and management of any concurrent health issues.
Appetite stimulants, such as mirtazapine, may be helpful for dogs not interested in eating.
A dog that has recovered from just a single episode of pancreatitis may develop extensive scarring within the pancreatic tissue.
Scarring of the pancreas can lead to the development of diabetes mellitus and/or a condition called exocrine pancreatic insufficiency (EPI).
Symptoms of pancreatitis in dogs are not specific to the pancreas—because of this, it can be a challenge to diagnose.
However, the earlier the diagnosis and treatment, the better the chance for recovery.
Prevention of Pancreatitis in Dogs
Most cases of pancreatitis are due to unknown causes, so it’s difficult to prevent.
However, because diet is linked to the development of pancreatitis, refraining from feeding your dog table scraps and high-fat foods reduces the risk of this condition.
Dogs with underlying health conditions, such as Cushing’s disease, are at an increased risk of pancreatitis.
Bringing your dog to follow-up appointments and giving medications as prescribed for chronic health conditions will reduce their risk for pancreatitis.
